Kenyan youth opt for HIV self-testing kits for fear of stigma
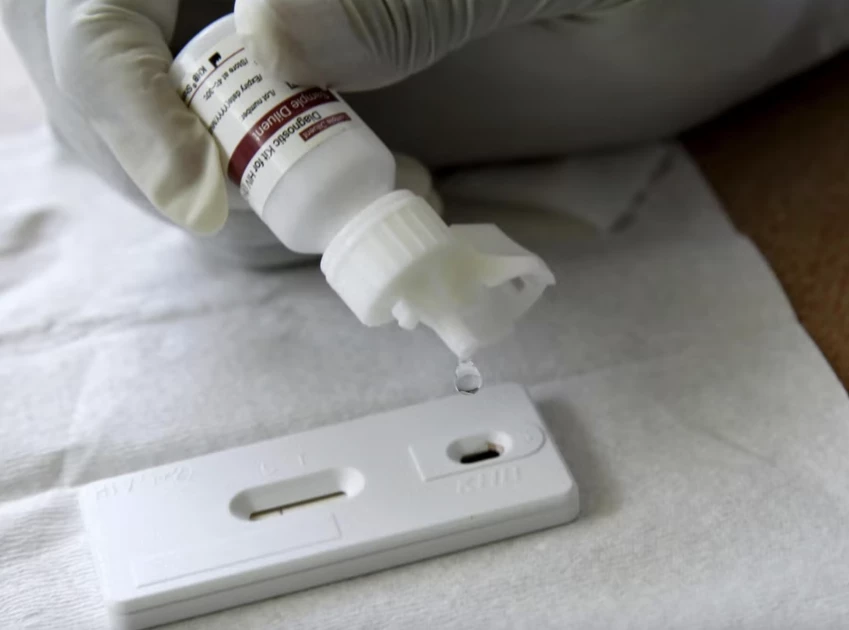
File photo: A reactor is added to a blood sample to test for HIV (REUTERS/Thomas Mukoya)

Audio By Vocalize
The world suddenly came to an abrupt end, for Maua (not her real name). How would she face and tell the world she is HIV (Human Immunodeficiency Virus) positive? She tried all things possible to remain calm without success.
In Grade Seven and HIV positive! She asked herself many questions about where she might have gone wrong. After a long struggle with what to, or not do with herself, Maua mustered enough courage and decided to let everything be, however bad it is.
“After all, we will all die one day one way or the other,” she consoled herself.
That was September 25, 2016, and Maua had just tested herself and discovered she had been infected with HIV. It all started when she started being sickly, time and again, that she decided to visit Migori Level 4 Hospital, to see what was ailing her.
Back to Maua, As they entered the hospital, accompanied by her fellow Grade Seven pupil, Maua opted for the self-test kit.
She feared if she got tested within the facility and was found positive, information might leak. If that were to happen, it would be hard to deal with the stigma associated with it.
She picked up her HIV self-testing kit and went back home. “The kit has all the instructions on how to test yourself, including showing whether one is negative or positive,” she shares.
HIV is a virus that attacks the body's immune system and if not treated, it can lead to AIDS (acquired immunodeficiency syndrome). There is currently no known cure but with proper medical care and the use of ARTs, HIV can be controlled.
Antiretroviral therapy or ART involves taking medicine prescribed by a health care provider which works to reduce the amount of HIV in your body.
As she prepared to do the test, Maua was worried about the outcome.
She says; “It is not easy when you are alone. Despite the fear of information of your status being known when you take a test at the facility, it is however much better there because there is a medical person to talk and counsel you.”
Though she lived with her aunt, Maua never revealed her status. She never even sought help from the hospital after knowing she was positive.
When she fell sick again and visited Kemo Valley Hospital for treatment that she discovered the facility was testing every patient for their HIV status.
She says they never sought her consent, but lied to her they were testing for diabetes. She recalls it was almost World AIDS Day held every year on December 1.
After they discovered she was positive, the facility contacted her aunt and shared Maua's HIV status.
“My aunt cried uncontrollably after learning of my HIV status,” remembers Maua who works as a volunteer for youths with HIV.
From here, Maua was directed to Ogembo Hospital, a public facility to start her antiretroviral treatment.
Like Maua, many youths have opted for the HIV self-testing kit, so that they can test themselves secretly for fear of their status being known to the public.
However, despite several interventions from the Ministry of Health, HIV spread is still a menace in the county.
The launch of HIV self-test kits by Nascop Kenya has bridged the diagnosis gap in HIV testing thereby reaching many people who cannot access HIV testing centres.
Since Migori County embraced the self-testing kit, supported by other interventions, there has been a notable decrease in its prevalence from 13.3 per cent in 2014 to 10.4 per cent according to the Kenya demographic survey.
Caroline Odera the Deputy County, Aids and STI Coordinator Migori, HIV Presentation Section explains most users of the test kits are adolescents and youths. But they are counselled first before they are handed self-testing kits.
She explains they target partners of pregnant mothers and breast-feeding mothers, to protect against mother-to-child infection.
“We give mothers self-test kits to take to their partners to test and know their status. In this, we are trying to reach men because they don’t go to hospital to seek medication,” she explains adding that another group they also target are adolescents, who also rarely visit hospitals.
Others on the list of targets are key populations; also at higher risk of contracting HIV like female sex workers, and men having sex with men, male sex workers, those who inject drugs and transgender.
She explains most of the services are offered in hospitals but men or key populations prefer outreach workers.
Odera regrets pregnant women who refuse to take the test-kits to their spouses because HIV testing is associated with gender-based violence.
“Women fear taking the test kits to their husbands, because the first question will be they don’t trust them, or if they are already infected, a reason they want them tested,” explains Odera.
Another youth who prefers self-testing kits over physical tests in a facility is Mary Adhiambo, from Awendo. When she got involved in unprotected sex, she opted for self-test kit, which she learned through a friend.
She recalls the incident that led her to unprotected sex, a few months ago.
“A male friend invited me out for coffee in Migori town. We had fun and by the time l decided to leave it was already late l couldn’t find means of transport back home, in Awendo,” she narrates.
Stranded, Adhiambo explains, her friend booked a guestroom. She tried to resist but her friend assured her nothing was going to happen between the two. However, in the dead of the night, the male friend changed and started demanding sex.
She explains, “At first, he appeared polite to which l said wasn’t ready for it. After some time, he changed and demanded. It looked like he was going to force me into sex if l continued resisting. Realising how helpless l was, just decided to cooperate and at this point asked if he had protection. He did not.”
Come morning, Adhiambo wanted them to go for an HIV test, He did not want to hear anything to do with the HIV test.
However, she was determined to know her fate, Adhiambo visited a local facility where she was admitted for Post-Exposure Prophylaxis (PEP) to prevent HIV after a possible exposure for 30 days.
Luckily, the HIV test turned negative. She was still not convinced and after 30 days on PEP, she went for another test again. She bought a self-test kit from a nearby chemist and tested herself. It was negative. She explains that she is lucky the test turned out negative.
Migori County received the last consignment of 8,100 self-test kits in the month of March last year and distributed them to target groups but only 3,000 returned the results to hospitals.
The HIV Estimates Report shows between 2014 and 2021, more than 57% of HIV infections are said to occur in eight of 47 counties which include; Migori, Kisumu, Siaya, Homa Bay, Kisii, Nakuru, Nairobi and Mombasa with key populations accounting for 30% of the new infections.
The rising cases of HIV infections have seen other stakeholders join hands with the government through the National AIDS and STIs Control Programmes NASCOP to complement and promote the use of self-test kits and other self-care products. Among those working with the government is Population Services International (PSI).
Serah Malaba, the PSI Project Director for the Strengthening HIV Self-Testing project in the Private Sector (SHIPS) that started in November 2020 says the aim of this project is to grow the private sector market for Hiv self-testing with a public health impact.
The project is sponsored by Children’s Investment Fund Foundation.
“We want to use HIV self-testing not only to find individuals who are already living with HIV so they can be put on treatment," she says.
"We also want to ensure that HIV self-testing becomes a way of life and a preventive measure to individuals engaging in sexual activities to enable them to continuously test them as per national guidelines."
Malaba explains that HIV testing or knowledge of someone’s status is the entry point and precondition to accessing effective HIV prevention care and treatment services.
The piloting project for PSI is taking place in Kisumu and Nairobi because they are among the eight counties that account for the highest number of new HIV infections.
She adds that they have rolled out a self-care driven campaign that features and positions HIV self-testing as part of HIV prevention, sexual reproduction health and HIV treatment programme.
They have also improved access to HIV self-testings and have positioned the pharmacist as an option where you can access not only HIV self-testing kits and also other sexual reproductive health products like condoms.
She observes; “We have also seen a lot of people buying emergency contraceptive pills, this shows people are engaging in unprotected sex. We have told the pharmacist to ensure that when someone comes in to buy emergency pills, they advise them about knowing their HIV status, buying HIV self-test kits, condoms and potentially considering long-term family planning options so that they don’t overuse the emergency pills.”
Malaba says they have engaged over 100 pharmacists in Kisumu and Nairobi.
Between April and November, the PSI sold 40,000 HIV testing kits.
According to the World Health Organization (WHO), there are 1.4 million people in Kenya living with HIV in 2021.
Globally, 38.4 million people are living with HIV with 19.7 million being women, 16.7 million being men and 1.7 million being children.

Leave a Comment